Res Dev Med Educ. 13:10.
doi: 10.34172/rdme.33188
Original Article
The effect of the feedback method on the obstetrics-gynecology residents’ learning in the management of early postpartum hemorrhage
Mahnaz Boroumand Rezazadeh Conceptualization, Data curation, Project administration, Resources, Writing – original draft, 1 
Tina Zeraati Investigation, Writing – original draft, 2, 3
Seyed Reza Mousavi Conceptualization, Project administration, Supervision, Writing – review & editing, 4
Nayereh Ghomian Conceptualization, Supervision, Writing – review & editing, 1
Leyli Hafizi Conceptualization, Supervision, Writing – review & editing, 1
Tayebeh Seyfizadeh Data curation, Investigation, Writing – original draft, 5
Mona Najaf Najafi Methodology, Writing – review & editing, 6
Majid Khadem-Rezaiyan Methodology, Software, Writing – review & editing, 7, 6, * 
Author information:
1Department of Obstetrics and Gynecology, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
2Medical Genetics Research Center, Mashhad University of Medical Sciences, Mashhad, Iran
3Kidney Transplantation Complications Research Center, School of Medicine, Mashhad University of Medical Science, Mashhad, Iran
4Medical Toxicology Research Center, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
5Department of Medical Education, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
6Department of Community Medicine and Public Health, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
7Medical Sciences Education Research Center, Mashhad University of Medical Sciences, Mashhad, Iran
Abstract
Background:
Simulation training, a novel learning method, provides medical students with opportunities to practice managing stressful situations as if they were experiencing them in reality. Recently, there has been increased recognition of the value of simulation-based education. This study aimed to evaluate the most effective approach for providing feedback during a simulation program.
Methods:
In this interventional study, a total of 43 obstetrics and gynecology residents were recruited and stratified into three groups based on their residency stage. These residents participated in a simulation-based program focused on the management of post-partum hemorrhage (PPH). The program involved handling a PPH scenario, during which they received feedback either during the task (in-task; IT) or after completing the task (end-task; ET). Following the simulation, a post-test was administered, and the results were compared between the IT and ET feedback groups.
Results:
Demographic variables did not differ significantly between the ET and IT groups. Generally, there were no significant differences in secondary knowledge (P=0.232) or secondary performance (P=0.196) following the simulation program between the two groups. However, Among second-year residents, the change in primary and secondary performance was not significant in either the ET (P=0.76) or IT (P=0.74) group, while the IT group showed a significant improvement in knowledge (P=0.04). For third-year residents, the point change in primary and secondary knowledge and performance was not statistically significant in either the ET or IT groups.
Conclusion:
The final knowledge and performance following simulation programs do not significantly differ between the IT and ET groups. However, second-year residents experienced an improvement in knowledge.
Keywords: Simulation, Resident, Learning
Copyright and License Information
© 2024 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, as long as the
original authors and source are cited. No permission is required from the authors or the publishers.
Funding Statement
This study (ID:971827) was registered at and supported by Mashhad University of Medical Sciences.
Introduction
The methods of education tend to be more practical, team-based, and similar to real life in higher educational levels, i.e. various specialty or subspeciality fields.1-5 Among these trends is the affinity towards replacing mainstream lecture-based educational methods with novel student-centered ones, such as simulation-based learning (SBL). Particularly, it is believed that SBL may play a crucial role in regards to the training of health care staff, including nurses and medical students, aiming to arm them with the essential performance in a secure situation, resembling real-life dangerous conditions.6,7 The profound impact of SBL on nursing education was noted by Kim et al.8 Villanueva et al9 reviewed the articles evaluating the SBL method. The research showed that although SBL methods are not addressed in the educational curriculum of medical students yet, they may result in an enhanced level of education and performance among medical students especially concerning surgery. As suggested by Aebersold,10 not only SBL appears to be an appropriate add-on method, but it also must be considered as a main part of the educational curriculum due to its short-term and long-term advantages, as well as the variety of learning options. Moreover, the wide spectrum of options to run a simulation program, in addition to the importance of appropriate feedback was highlighted within their study. The term “feedback”, defined as the information provided on different aspects of the student’s understanding or performance is an important issue in the SBL method, leading the students to a better overview of their negative and positive points.11 Correspondingly, they can improve the positive and reduce the negative aspects in the future.
In 2017, Sultan et al12 reviewed the positive aspects of giving feedback on both trainer and trainee. For instance, by trying to provide efficient feedback at the correct time using respectful and effective words, trainees can use the feedback-giving process as an opportunity for self-development. On the other hand, appropriate feedback will stop students from judging themselves inappropriately, thereby allowing them to set realistic goals to enhance their potentialities along with improving their weak points. Furthermore, as one of the trainers’ roles (i.e. facilitator13), a positive relationship between trainees and trainers can result from the process of giving and receiving feedback.14
Various feedback approaches have been discussed in the literature to investigate the most effective feedback strategy.15 Various methods have been suggested to classify feedback. The most trending classification strategy describes feedback in 3 groups: positive, negative, and blank feedback. The evaluation of feedback strategies in groups of in-task (IT) feedback which is given during the task, and end-task (ET) feedback which is given at the end of the performance is also noted in the literature. The pros and cons of each strategy have been broadly discussed in the literature. Nevertheless, the results are controversial. The current study was conducted to make a comparison between the two feedback-giving options, including IT and ET approaches.
Methods
Participants
The interventional study was conducted on 43 obstetrics and gynecology residents in Omolbanin, Imam Reza, and Ghaem hospitals of Mashhad, Iran. These are three tertiary academic hospitals affiliated with Mashhad University of Medical Sciences.
The inclusion criteria were being a resident of obstetrics and gynecology at Mashhad University of Medical Sciences. The exclusion criteria were reluctance to participate in this study or incomplete checklists ( > 20% of questions). They were stratified into 3 separate groups based on their residency year; second year (n: 15), third year (n: 14), and fourth-year (n: 15) residents. Their demographic characteristics, including age and marital status, were recorded, in addition to their primary educational condition according to the points they had earned in their routine exams and the residency entrance exam.
Sources
The management of post-partum hemorrhage was trained based on the UpToDate 2020 database, the national protocol of post-partum hemorrhage management updated in 2017,16 and the Williams obstetrics & gynecology book published in 2018.17
Assessment
First, the participants were given a descriptive test emphasizing the management of post-partum hemorrhage, and their performance was rated through an objective structured clinical examination (OSCE) with the same topic (post-partum hemorrhage, PPH)18; the scores were recorded. The maximum point for the OSCE exam was 50, and the maximum point concerning the descriptive test was 10. Then, the students were asked to watch a recorded lecture in terms of essential points about the management of PPH. After a week, the students were given a descriptive test; similar to the previous one, and the points were recorded. In the next step, students in each group were randomized into 2 equal groups of IT feedback and ET feedback. The participants in each group were asked to join separate simulation programs, in which they had the opportunity to manage a scenario of PPH under the observation of an instructor for 20 minutes. The instructor was responsible for assessing their performance and giving them feedback. The feedback was given to the IT groups during their performance, while the ET groups were given feedback at the end. One month later, their abilities to manage the PPH were interfered with using a descriptive test and an OSCE.
Statistical analysis
The results were compared between groups and within each group using SPSS 26. The normality of the variables was confirmed using Kolmogorov–Smirnov test. Continuous and categorical variables were presented as mean ± > SD, and frequency (percentage), respectively. Inter-group comparisons were performed using the independent Student’s 𝑡-test for normally distributed variables. Intra-group comparisons were performed with a paired sample t-test. Categorical variables were compared using the Chi-square (χ2). All tests were two-tailed and a P value < 0.05 was considered statistically significant.
Results
There were no significant differences in demographic variables between the IT and ET groups. Our results showed that although the points received by the ET group seemed better, the point differentiation was not superior to the IT group, before and after the simulation program (Table 1). On the other hand, our data analysis revealed that our SBL program has resulted in a significant rise in the level of knowledge and performance in all groups compared to their primary knowledge and performance level (P < 0.001). Considering the year of residency as the effect-modifier variable, we compared the differentiation between the primary and secondary knowledge and performance amongst the 3 groups consisting of residents in the second, third, and fourth year of their residency. Our results suggested the superiority of improving knowledge in the IT group amongst 2nd year residents (P = 0.04), and the improvement of performance in the third-year residents in both IT (P = 0.07) and ET group (P = 0.06) (Table 2, Figure 1).
Table 1.
Comparison of demographic features and primary and secondary levels of knowledge and performance between study groups
|
|
IT Group
|
ET group
|
P
value
|
| Age (years) |
32.4 ± 3.3 |
34.7 ± 4.9 |
0.175 |
| Marital status |
|
|
|
| Single |
6 (31.6%) |
2(11.8%) |
0.236 |
| Married |
13 (68.4%) |
15 (88.2%) |
| The gap between being a general practitioner and residency (year) |
6.3 ± 3.3 |
7.8 ± 3.3 |
0.107 |
| Score of the residency entrance exam (of 600) |
346.1 ± 13.9 |
353.1 ± 11.0 |
0.186 |
| Primary knowledge (points) |
2.9 ± 2.0 |
3.0 ± 1.3 |
0.573 |
| Primary performance (points) |
15.6 ± 5.7 |
15.9 ± 4.1 |
0.925 |
| Secondary knowledge (points) |
5.2 ± 2.7 |
6.5 ± 2.1 |
0.232 |
| Secondary performance (points) |
28.1 ± 8.6 |
31.7 ± 5.7 |
0.196 |
Data represented as mean ± standard deviation or frequency (percentage).
Table 2.
Comparison of primary and secondary knowledge and performance amongst residents based on year of residency
|
Domain
|
Group
|
Assessment
|
2nd Residency year
|
3rd Residency year
|
4th Residency year
|
| Knowledge |
ET group |
Primary |
2.5 ± 1.0 |
2.3 ± 0.5 |
3.8 ± 1.5 |
| Secondary |
5.2 ± 2.2 |
5.9 ± 1.7 |
7.9 ± 2.0 |
|
P value |
0.49 |
0.21 |
0.51 |
| IT group |
Primary |
2.0 ± 1.4 |
3.6 ± 2.8 |
3.0 ± 1.08 |
| Secondary |
4.1 ± 2.4 |
4.6 ± 2.7 |
6.3 ± 2.7 |
|
P value |
0.04 |
0.26 |
0.52 |
| Performance |
ET group |
Primary |
15.8 ± 1.7 |
14.0 ± 3.9 |
17.6 ± 4.8 |
| Secondary |
27.0 ± 4.9 |
33.6 ± 2.6 |
32.7 ± 7.0 |
|
P value |
0.76 |
0.06 |
0.79 |
| IT group |
Primary |
17.4 ± 2.4 |
17.6 ± 3.3 |
13.1 ± 7.7 |
| Secondary |
30.0 ± 7.3 |
25.1 ± 10.6 |
29.1 ± 8.1 |
|
P value |
0.74 |
0.07 |
0.78 |
Data represented as mean ± standard deviation and compared with paired sample t-test.
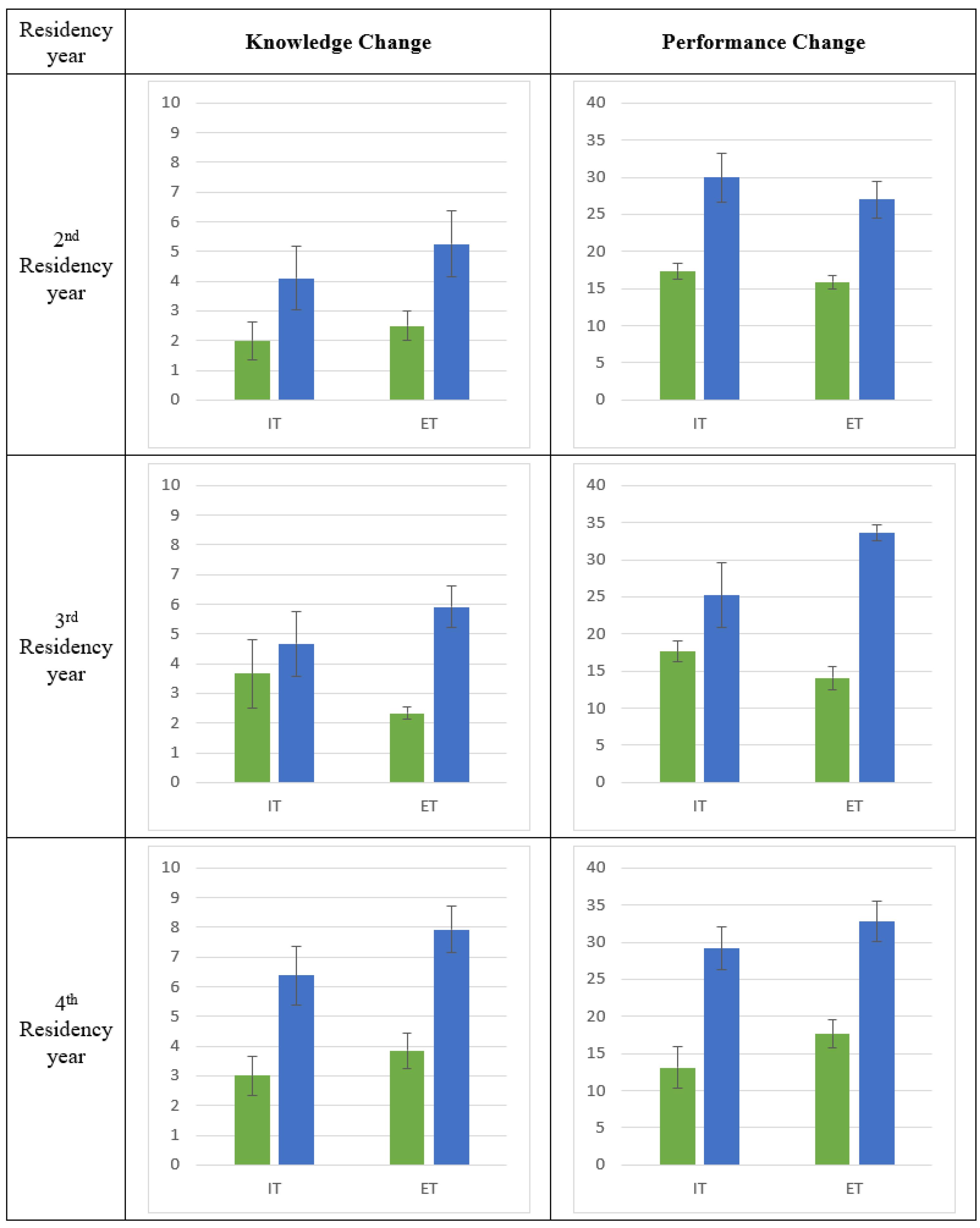
Figure 1.
Knowledge and performance change in each group (IT: in-task feedback; ET: end-task feedback). Primary and secondary assessments are shown in green and blue color, respectively. Error bars = 1 SE
.
Knowledge and performance change in each group (IT: in-task feedback; ET: end-task feedback). Primary and secondary assessments are shown in green and blue color, respectively. Error bars = 1 SE
Discussion
This study aimed to compare the effectiveness of IT feedback versus ET feedback within the context of a SBL program. The primary objective was to train obstetrics and gynecology residents in the management of PPH.
Generally, the results suggested no significant difference between the two methods. However, a slight improvement in knowledge was observed in the 2nd year IT group, as well as a minor improvement in performance in both IT and ET 3rd year residents.
Feedback is described as a dynamic process, in which both learners and clinical supervisors are involved so that the students can be informed about the quality of their performance and its negative and positive aspects. Research shows that the students may benefit from proper feedback emphasizing their necessities, to identify their strengths and weaknesses.19,20 Numerous research studies have appraised the impact of feedback in medical education. Yet, the literature seems to lack clinical trials to compare the effect of various types of feedback. Various categorizations have been suggested to date for feedback, including formal and informal, negative, and positive, IT and ET, directive and facilitative, and so on. Chawes and Johannesen21 compared two types of feedback described as summative and formative. Formative feedback is ongoing, and it is given during educational courses, while summative feedback is usually given at the end of a career, as if the trainer sums up what the trainees have learned. It seems that the meaning of formative feedback is so close to IT feedback, while summative feedback is defined likewise the ET feedback in our study. However, they do not exactly share the same meaning. IT and ET classification refers to a single task while formative and summative are usually used to assess a career. Lean et al22 conducted a study to compare both long-term and short-term retention of information in following SBL programs associated with either IT feedback or ET feedback; their results suggested that ET feedback provides significantly better promotion of both long-term and short-term retention for medical students. Jug et al23 reviewed the importance of feedback in medical education. They described the barriers to giving and receiving feedback. As they suggested, receiving feedback is as important as giving it. The trainees should try to enhance their listening skills and decision-making. They should be aware that not only does not negative feedback humiliate them at all, but also helps them identify their weak points so that they can plan to find an appropriate solution.
In the study conducted by Roberts et al24 in 2017, the effect of per-assessment during a collaborative activity was evaluated. According to their results, although peer feedback is likely to improve their decision-making skill, it may cause an interruption in assessing the individuals in the team. Hence, supervisors should not decide about students’ scores by looking at their response to feedback during the performance in the team. Lerchenfeldt et al25 in 2019, introduced some limitations and advantages of giving peer feedback. Their results suggested that peer feedback is usually followed by positive outcomes. On the other hand, inappropriate feedback can be disruptive, because it makes the class environment undesirable. Such an environment may result in an increased level of stress in association with reduced quality of interpersonal communication. Suhoyo et al26 conducted a study to compare the effectiveness of group feedback versus individual feedback in medical education. They asked 215 medical students to fill out a survey, emphasizing the characteristics and outcomes of whether individual feedback or group feedback received in 2 weeks. Their results showed that group feedback usually cause the development of students’ performance, while individual feedback more often insist on correcting the performance deficiencies. Their results also demonstrated that group feedback more often leads to making plans of action than individual feedback does. The conclusion may be related to the desire of the whole team to achieve their goals. That they only focused on students’ perceptions instead of learning outcomes seems to be a limitation of their study.
In 2020 a group of researchers from 17 medical faculties in Germany, Switzerland, and the Netherlands came together and held a workshop, discussing the feedback-giving strategies in medical education. The results of their discussion suggested that feedback given focusing on the process and performance during the task is as important as the feedback given on the results at the end of the process; moreover, appropriate feedback can enhance the student-teacher relationship. Their findings are in line with ours.27 Mueller et al28 assessed the differences between the feedback that male and female emergency medicine residents received from their attending physicians. Their results suggested a significant gender bias in medical education.
The results of our supplementary analysis by repeated measure test suggested that the performance improvement through the SBL method is more considerable in the third-year residents. It may result from the extraordinary desire to improve performance in this group compared to the 2nd year residents who still lack enough theory information, thereby not being capable of using the insufficient knowledge to enhance their performance. On the other hand, 4th year residents have already reached their needed level of knowledge and performance; therefore, they are not motivated for promotion. Hence, it is recommended that further studies be done using a study population emphasizing this group so that more valuable results will be achieved, using fewer financial and human resources.
A notable strength of our study was that all of our study groups were under the observation of the same trainer. Moreover, the students were assessed in different groups according to their residency year, therefore the level of their knowledge in each group seemed to be equal. Another strength of our study was our focus on the documented learning outcomes instead of the personal notions. Additionally, the performance in our study was rated through a formative OSCE. According to the literature, not only the OSCE is considered a reliable tool to evaluate learners` capabilities, but also it is associated with positive outcomes. For example, Luo et al29 in 2022, demonstrated that a formative OSCE with immediate feedback can significantly improve surgical clerks’ self-confidence as well as their clinical competence concerning several educational and psychiatric goals.
The main limitation of our study was the conditions associated with the COVID-19 pandemic, which caused some limitations in holding more qualified collaborative programs with a larger study population. In addition, only female residents participated in our study; it is recommended that the same process be performed in the future using a larger study population in different majors consisting of both male and female students.
Conclusion
The evidence suggests that the learning outcomes of an educational program using the SBL method do not significantly differ among students who received either IT or ET feedback. Furthermore, SBL appears to be one of the most preferred methods for enhancing the performance level of medical students.
Acknowledgments
The authors appreciate the support of the Medical Sciences Education Research Center for cooperation in preparing and revising this manuscript. They also appreciate the support of the Vice Chancellor for Research at Mashhad University of Medical Sciences.
Competing Interests
The authors declared no conflict of interest.
Ethical Approval
The Ethics Committee of Mashhad University of Medical Sciences approved this study (IR.MUMS.REC.1399.157).
References
- Fakouri E, Keshmiri F. Formative evaluation through case-based discussion method in gynecological diseases internship. Horizon of Medical Education Development 2022; 12(4):73-64. doi: 10.22038/hmed.2020.52386.1088.[Persian] [Crossref] [ Google Scholar]
- Soltani M, Amini M, Milani N, Hashemzadeh k, Ganji A, Lotfi Z. The effect of virtual distance learning on physical examination competency of internal medicine residents. Horizon of Medical Education Development 2021; 12(3):50-8. doi: 10.22038/hmed.2020.51895.1083.[Persian] [Crossref] [ Google Scholar]
- Allahyari A, Mohebbi M, Farzanehfar M, Abbasi Shaye Z, Akbarirad M, Goshayeshi L. Evaluation of the satisfaction of residents of the Internal medicine department of Mashhad University of Medical Sciences from combined education (virtual and face-to-face) in 2020. Horizon of Medical Education Development 2022; 13(2):18-6. doi: 10.22038/hmed.2021.55694.1129.[Persian] [Crossref] [ Google Scholar]
- Bashardoust N, Rezvan F, Maroufizadeh S, Mirfarhadi N. Characteristics of effective teaching based on the postgraduate dental students’ viewpoints in Iranian medical sciences universities in 2021. Horizon of Medical Education Development 2023; 14(1):15-5. doi: 10.22038/hmed.2021.59534.1169.[Persian] [Crossref] [ Google Scholar]
- Ghiyasvandian S, Haji Mohamad HoseiniM, Asayesh H, Sadeghi R, Azadeh M, Parvaresh Masoud M. The effect of team-based learning on students’ learning and motivation of students of medical emergency in the triage lesson. Horizon of Medical Education Development 2021; 12(1):43-34. doi: 10.22038/hmed.2020.50081.1053.[Persian] [Crossref] [ Google Scholar]
- So HY, Chen PP, Wong GK, Chan TT. Simulation in medical education. J R Coll Physicians Edinb 2019; 49(1):52-7. doi: 10.4997/jrcpe.2019.112 [Crossref] [ Google Scholar]
- Lee J, Lee H, Kim S, Choi M, Ko IS, Bae J. Debriefing methods and learning outcomes in simulation nursing education: a systematic review and meta-analysis. Nurse Educ Today 2020; 87:104345. doi: 10.1016/j.nedt.2020.104345 [Crossref] [ Google Scholar]
- Kim J, Park JH, Shin S. Effectiveness of simulation-based nursing education depending on fidelity: a meta-analysis. BMC Med Educ 2016; 16:152. doi: 10.1186/s12909-016-0672-7 [Crossref] [ Google Scholar]
- Villanueva C, Xiong J, Rajput S. Simulation-based surgical education in cardiothoracic training. ANZ J Surg 2020; 90(6):978-83. doi: 10.1111/ans.15593 [Crossref] [ Google Scholar]
- Aebersold M. Simulation-based learning: No longer a novelty in undergraduate education. Online J Issues Nurs 2018; 23(2):39. doi: 10.3912/OJIN.Vol23No02PPT39 [Crossref] [ Google Scholar]
- Toale C, Morris M, Kavanagh DO. Perspectives on simulation-based assessment of operative skill in surgical training. Med Teach 2023;45(3):313-20.. 10.1080/0142159x.2022.2134001.
- Sultan AS, Mateen Khan MA. Feedback in a clinical setting: a way forward to enhance student’s learning through constructive feedback. J Pak Med Assoc 2017; 67(7):1078-84. [ Google Scholar]
- Nili Ahmadabadi MR, Mohtadi S. Educational agent’s role and learning. Horizon of Medical Education Development 2021; 12(2):105-97. doi: 10.22038/hmed.2020.51649.1081.[Persian] [Crossref] [ Google Scholar]
- Jani MR, Barzegari Z, Razmara M, Nikkhah Beydokhti A, Gharib H, Dastgerdi G. The viewpoint of clinical students and trainers in Qaen school of nursing and midwifery about facilitating and inhibiting factors in clinical skills learning. Horizon of Medical Education Development 2022; 12(4):84-74. doi: 10.22038/hmed.2020.52169.1087.[Persian] [Crossref] [ Google Scholar]
- Brookhart SM. How to Give Effective Feedback to Your Students. Alexandria, VA: Association for Supervision and Curriculum Development (ASCD); 2017.
- The National Protocol of Post-Partum Hemorrhage Management. The Bureau of Standardization and Preparing Clinical Guidelines, Iranian Ministry of Health and Medical Education. 2017. Available from: https://med.mui.ac.ir/sites/med/files/users/darmanmed/After_delivery_bleeding_0.pdf. Accessed January 1, 2024.
- Cunningham, F. Gary, ed. Williams Obstetrics. 25th ed. New York: McGraw-Hill; 2018.
- Tavakol M, Scammell BE, Wetzel AP. Feedback to support examiners’ understanding of the standard-setting process and the performance of students: AMEE Guide No 145. Med Teach 2022; 44(6):582-95. doi: 10.1080/0142159x.2021.1993164 [Crossref] [ Google Scholar]
- Spooner M, Duane C, Uygur J, Smyth E, Marron B, Murphy PJ. Self-regulatory learning theory as a lens on how undergraduate and postgraduate learners respond to feedback: a BEME scoping review: BEME Guide No 66. Med Teach 2022; 44(1):3-18. doi: 10.1080/0142159x.2021.1970732 [Crossref] [ Google Scholar]
- Kuhlmann Lüdeke A, Guillén Olaya JF. Effective feedback, an essential component of all stages in medical education. Universitas Medica 2020; 61(3):32-46. doi: 10.11144/Javeriana.umed61-3.feed [Crossref] [ Google Scholar]
- Chawes B, Johannesen J. [Feedback loops in medical education]. Ugeskr Laeger 2020; 182(30):V03200176. [ Google Scholar]
- Lean LL, Hong RYS, Ti LK. End-task versus in-task feedback to increase procedural learning retention during spinal anaesthesia training of novices. Adv Health Sci Educ Theory Pract 2017; 22(3):713-21. doi: 10.1007/s10459-016-9703-8 [Crossref] [ Google Scholar]
- Jug R, Jiang XS, Bean SM. Giving and receiving effective feedback: a review article and how-to guide. Arch Pathol Lab Med 2019; 143(2):244-50. doi: 10.5858/arpa.2018-0058-RA [Crossref] [ Google Scholar]
- Roberts C, Jorm C, Gentilcore S, Crossley J. Peer assessment of professional behaviours in problem-based learning groups. Med Educ 2017; 51(4):390-400. doi: 10.1111/medu.13151 [Crossref] [ Google Scholar]
- Lerchenfeldt S, Mi M, Eng M. The utilization of peer feedback during collaborative learning in undergraduate medical education: a systematic review. BMC Med Educ 2019; 19(1):321. doi: 10.1186/s12909-019-1755-z [Crossref] [ Google Scholar]
- Suhoyo Y, Schönrock-Adema J, Emilia O, Kuks JB, Cohen-Schotanus J. Clinical workplace learning: perceived learning value of individual and group feedback in a collectivistic culture. BMC Med Educ 2018; 18(1):79. doi: 10.1186/s12909-018-1188-0 [Crossref] [ Google Scholar]
- Thrien C, Fabry G, Härtl A, Kiessling C, Graupe T, Preusche I. Feedback in medical education - a workshop report with practical examples and recommendations. GMS J Med Educ 2020; 37(5):Doc46. doi: 10.3205/zma001339 [Crossref] [ Google Scholar]
- Mueller AS, Jenkins TM, Osborne M, Dayal A, O’Connor DM, Arora VM. Gender differences in attending physicians’ feedback to residents: a qualitative analysis. J Grad Med Educ 2017; 9(5):577-85. doi: 10.4300/jgme-d-17-00126.1 [Crossref] [ Google Scholar]
- Luo P, Shen J, Yu T, Zhang X, Zheng B, Yang J. Formative objective structured clinical examination with immediate feedback improves surgical clerks’ self-confidence and clinical competence. Med Teach 2023; 45(2):212-8. doi: 10.1080/0142159x.2022.2126755 [Crossref] [ Google Scholar]