Res Dev Med Educ. 13:7.
doi: 10.34172/rdme.33210
Original Article
A Holistic Model of Organizational Trust with the Approach of Professional Ethics in Iranian Health System: A Case Study of the Universities of Medical Sciences in Iran
Mohammad Hossein Kashefi Conceptualization, Data curation, Investigation, Resources, Software, Writing – original draft, Writing – review & editing, 1 
Nader Bohlooli Project administration, Supervision, 2, * 
Karim Eskandari Investigation, Methodology, Software, 3 
Hossein Emari Resources, 2 
Author information:
1Student in Public Administration - Human Resource Management, Bonab Branch, Islamic Azad University, Bonab, Iran
2Department of Public Administration, Bonab Branch, Islamic Azad University, Bonab, Iran
3Department of Public Administration, Payam Noor University, Tehran, Iran
Abstract
Background:
Given the growing significance of trust and professional ethics within modern organizations, particularly in universities of medical sciences and educational institutions tasked with safeguarding public health, this study aimed to introduce an inclusive organizational trust model utilizing a professional ethics framework within the healthcare system.
Methods:
The research method of this study was a cross-sectional survey of 240 managers, experts, and employees of the health system. The data collection tool was a questionnaire whose validity and reliability have been checked and confirmed using relative content validity ratio (CVR), content validity index (CVI), and Cronbach’s alpha. To analyze the data, confirmatory factor analysis and structural equation model with partial least squares (PLS) were used to test the model.
Results:
Based on the research findings (44.7%), the indicators related to cultural and ethical standards (R2=0.742), internal organizational standards (R2=0.689), organizational consequences (R2=0.758), and social consequences (R2=0.690) accentuate the desirability of endogenous structures within the model. The analysis revealed that all factor loadings’ t-values exceeded 1.96 at the 95% confidence level. Hence, a substantial association between manifest variables (concepts) and latent variables (categories) was established, with all factor loadings being validated. Specifically, environmental factors demonstrate the strongest influence on cultural and ethical standards (t=6.210), while structural domains exert a considerable effect on inter-organizational standards (t=4.614). Notably, inter-organizational standards exhibit the most substantial impact on both social consequences (0.407, t=6.813) and organizational outcomes (0.405, t=3.941). Overall, the findings demonstrated a positive and statistically significant impact of causal conditions on the central phenomenon, contextual, intervening, and central conditions on organizational strategies, as well as strategies on the outcomes of organizational trust within a framework of professional ethics in the healthcare sector.
Conclusion:
More attention and application of causal factors, contextual factors, intervening factors, and central factors increase the category of trust and professional ethics in organizations, especially the universities of medical sciences and medical training centers.
Keywords: Medical sciences institutions, Organizational trust, Professional ethics, Healthcare system
Copyright and License Information
© 2024 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, as long as the
original authors and source are cited. No permission is required from the authors or the publishers.
Funding Statement
This research did not receive any financial support from individuals or entities, whether natural or legal.
Introduction
The rise of globalization has underscored the crucial role of trust in social, political, economic, and organizational realms. Experts across various disciplines have highlighted trust as a cornerstone of organizational effectiveness. The healthcare system, being a critical sector dealing with the well-being of individuals and society as a whole, necessitates a high level of professional ethics and robust organizational trust amongst its personnel and management. Upholding professional ethics is innate to the healthcare and medical field, with the primary objective of delivering top-tier health, care, treatment, and rehabilitation services to safeguard, preserve, and enhance societal health standards.1 Trust, as defined by Pourhaydari et al,2 is a confidence between two parties that yield positive outcomes for both. In general, trust in organizational structure plays a crucial role in fostering coordination and participation, yielding numerous benefits such as promoting solidarity, fostering growth, enhancing work morale, reducing absenteeism, and fostering a sense of belonging within the organization. According to Saunders and Thornhill,3 optimal trust among organizational agents is achieved when all necessary structural elements are in place, and a cohesive blend of trust components is maintained. When employee trust is compromised, individuals may lose motivation to engage in trust-based behaviors like collaboration, voluntary contributions, knowledge sharing, and effective problem-solving, consequently hindering organizational performance. Moreover, unclear motives on the part of employers can lead to employee uncertainty,4 This lack of trust is particularly detrimental in critical sectors like healthcare, where organizational effectiveness directly impacts service recipients’ well-being. Achieving organizational goals hinges on seamless collaboration among all members, emphasizing the importance of fostering mutual trust among employees and between employees and management.5
On the other hand, while ethics are essential in all professions, they are especially critical in roles within the healthcare system. This is because the ethical and responsible conduct of employees toward patients significantly impacts the improvement and restoration of their health. Therefore, professions within the healthcare sector are fundamentally rooted in ethics.6
Today, it is widely acknowledged by many nations that disregarding moral considerations and evading social duties and responsibilities can result in the downfall of an institution.7
The fundamental essence of healthcare is grounded in the acknowledgment and preservation of human rights, encompassing the rights to life and autonomy, as well as the importance of dignity and respectful conduct. Adherence to ethical principles across various healthcare professions and practices results in enhanced service delivery. The enhancement of human resources quality plays a pivotal role in bolstering patient outcomes. Therefore, prioritizing these aspects is imperative within any organization, particularly those within the healthcare ecosystem, as highlighted by Salam et al in 2013.8
When transitioning from personal to professional spheres, various ethical codes come into play, such as medical, teaching, and engineering ethics. It can be perplexing to witness a hospital or university system embroiled in corruption while simultaneously expecting medical professionals or educators to uphold ethical standards. In the contemporary landscape, professional ethics play a crucial role within organizations, with strategic management experts emphasizing the importance of ethical principles as a foundation for effective management. Professional ethics entail both the moral obligations of the organization towards internal and external stakeholders, distinct from but inclusive of labor rights. Upholding sound ethical standards is pivotal in fostering a positive organizational culture, ultimately shaping a reputable company.9
Some of the previous studies conducted in this field are as follows:
In 2022, Atalay et al carried out a study entitled “The impact of perceived organizational support and organizational trust on the organizational commitment of young academics” at Turkish universities. The research revealed that perceived organizational support and organizational trust positively and significantly influence affective and normative commitment. Interestingly, the study also highlighted that trust in managers has a notable negative impact on continuance commitment.10
In 2022, Garib et al. conducted research entitled “Creating a model of factors influencing the development of professional ethics in nurses.” The findings revealed that culture, management style, education, personality traits, moral intelligence, and spiritual values are the most significant factors influencing the development of nursing professional ethics. From this, we can infer that the growth of professional ethics in both male and female nurses is not arbitrary. Factors such as ethical leadership, training, well-designed organizational systems and infrastructures, and open and effective communication grounded in organizational ethics are vital for motivating and encouraging progress in this area.11
Soni and Mehta conducted a research entitled “Explaining the internal social responsibility of companies on employee commitment: the mediating role of organizational trust” and the results show that the internal social responsibility practices of companies have a significant and positive effect on employee commitment. In addition, the mediating role of organizational trust was also confirmed.12
In their 2018 study entitled “Nurses’ trust and organizational goals for continued employment in Turkish hospitals,” Basit and Duygulu found that the trust level of nurses in their current workplace was low, while trust in their colleagues was high. Moreover, nurses who expressed satisfaction with their current workplace and intended to continue working there exhibited a high level of confidence.13
In a study entitled “Professional ethics in the organization” conducted by Bowen et al in 2016, the findings indicate that ethical and moral attributes play a crucial role in fostering trust within the organization. This ultimately enhances organizational processes and communication.14
In 2017, Haghgoo et al conducted research on “Designing a model for the development of professional ethics in government organizations within Iran’s health system.” Their findings indicate that the implementation of professional ethics in the healthcare sector necessitates the establishment of a structured and systematic process. They emphasize the importance of education, the creation of organizational structures, and the institutionalization of ethical standards, tailored to the specific conditions and needs of individual countries.15
In their 2016 study, Asadian et al explored the link between professional ethics, organizational trust, and psychological empowerment among teachers. The findings revealed a strong, positive correlation between professional ethics and its various facets, as well as psychological empowerment. Additionally, a significant association was observed between organizational trust and the psychological empowerment of teachers. The regression analysis further supported the existence of a linear relationship, indicating that professional ethics and organizational trust can be predictive factors for psychological empowerment.16
One of the main challenges in creating and maintaining trust in the health system is the increasing dynamism and complexity of this system. Today, the health system has become more complex due to advances in health care, medical technology, changes in patient demographics and expectations, and the increasing importance of collaboration and teamwork among health professionals. These factors have led to increased pressure on health organizations to improve performance and meet the diverse needs of patients and their families. In addition, the COVID-19 pandemic has revealed the vulnerabilities and limitations of the health system and emphasized the need for a comprehensive approach to address health challenges. Recent research has shown that it is necessary to establish trust and ethical standards to promote cooperation between health professionals and reduce conflicts and tensions, which ultimately improves the quality of services and ensures fair access to health services.
With the investigations carried out in previous research, it was found that various research studies have investigated the issue of organizational trust and professional ethics separately, but the simultaneous study of the two variables of professional ethics and organizational trust in the health system has not been the focus of researchers. The lack of a suitable model for creating organizational trust based on professional ethics based on the values and standards of Iran’s government organizations prompted the researchers of this research to take steps in this field. This research, while simultaneously paying attention to these two variables, seeks to develop and present a comprehensive model of organizational trust using the results of past research with two categories: localization and adaptation, with dimensions, components, and indicators that are suitable for Iran’s health system.
Methods
This study employs a cross-sectional survey methodology for data collection within the Iranian health system. The target population includes all managers, experts, and employees working within that system. A researcher-designed questionnaire was used to gather data. This questionnaire was informed by a previous qualitative study that utilized a grounded theory approach for analysis. Participant responses were assessed on a five-point Likert scale (very low to very high).
To ensure the appropriateness of the questionnaire, content validity was assessed by consulting 10 experts in the field of management. Their feedback was weighted and a validity score was calculated using a standard formula. Additionally, the questionnaire’s internal consistency was determined by calculating Cronbach’s alpha.
The questionnaire comprises 87 questions organized into these categories: Causal conditions (11 questions), contextual factors and formation platform (18 questions), intervening conditions (8 questions), strategies for establishing organizational trust (23 questions), consequences of organizational trust (25 questions), and central phenomenon factor (2 questions), focused on organizational trust based on professional ethics.
Structural equation modeling (SEM) with partial least squares (PLS) software was used for analysis. Following Haire’s17 guidelines, a minimum sample size of 240 was determined based on the number of observable variables in the model (15 × 16 = 240). The most obvious variable related to the causal factors is the number of 16 variables, and for each obvious variable, 15 samples are selected and the research questionnaire is determined.
As a result, 240 questionnaires were collected and analyzed from the statistical population. Descriptive and inferential statistical methods were then utilized to analyze the data obtained. The descriptive findings and the percentage of responses related to the questionnaire questions and research variables were presented. At the inferential level, to test the research hypotheses and the presented model, structural equations were utilized with the PLS method.
Results
The descriptive findings from the 240 respondents who completed the research questionnaires indicated that 159 (66.3%) were male. In terms of age distribution, the largest group consisted of 92 (38.4%) between the ages of 30 and 40, while 16 (6.6%) were under the age of 30. Regarding educational qualifications, the majority held bachelor’s degrees, totaling 157 (65.5%), while those with post-graduate degrees and below accounted for only 22 (9%). Considering work experience, 107 (44.7%) had 10 to 20 years of experience, and 29 (12.2%) had less than 10 years of experience. Table 1 provides an overview of the demographic characteristics of the sample under study.
Table 1.
Quantity and frequency of analyzed samples
|
Variable
|
No. (%)
|
| Gender |
Male |
159 (66.3) |
| Female |
81 (33.7) |
| Education |
Associate degree and below |
22 (9.0) |
| Bachelor's degree |
157 (65.5) |
| Master’s degree and higher |
61 (25.5) |
| Age |
Less than 30 |
16 (6.7) |
| Between 30-40 |
92 (38.4) |
| Between 40-50 |
89 (36.9) |
| Over 50 |
43 (0.18) |
| Work experience |
Less 10 years |
29 (12.2) |
| Between 10-20 years |
107 (44.7) |
| Over 20 years |
104 (43.1) |
| Total |
240 (100) |
In this study, Smart PLS software utilized SEM based on PLS to address research questions and assess the validity and reliability of indicators. The partial least squares technique was employed to validate the model. The results obtained from running the model in standard estimation mode provide insights into the direction and strength of relationships between variables, as indicated by factor loadings A higher factor loading value for an indicator concerning a specific construct indicates the greater explanatory role of that indicator in the construct. Conversely, a negative factor loading suggests a negative impact on the related construct. The output generated by Smart PLS software for standard estimation can be observed in Figure 1.
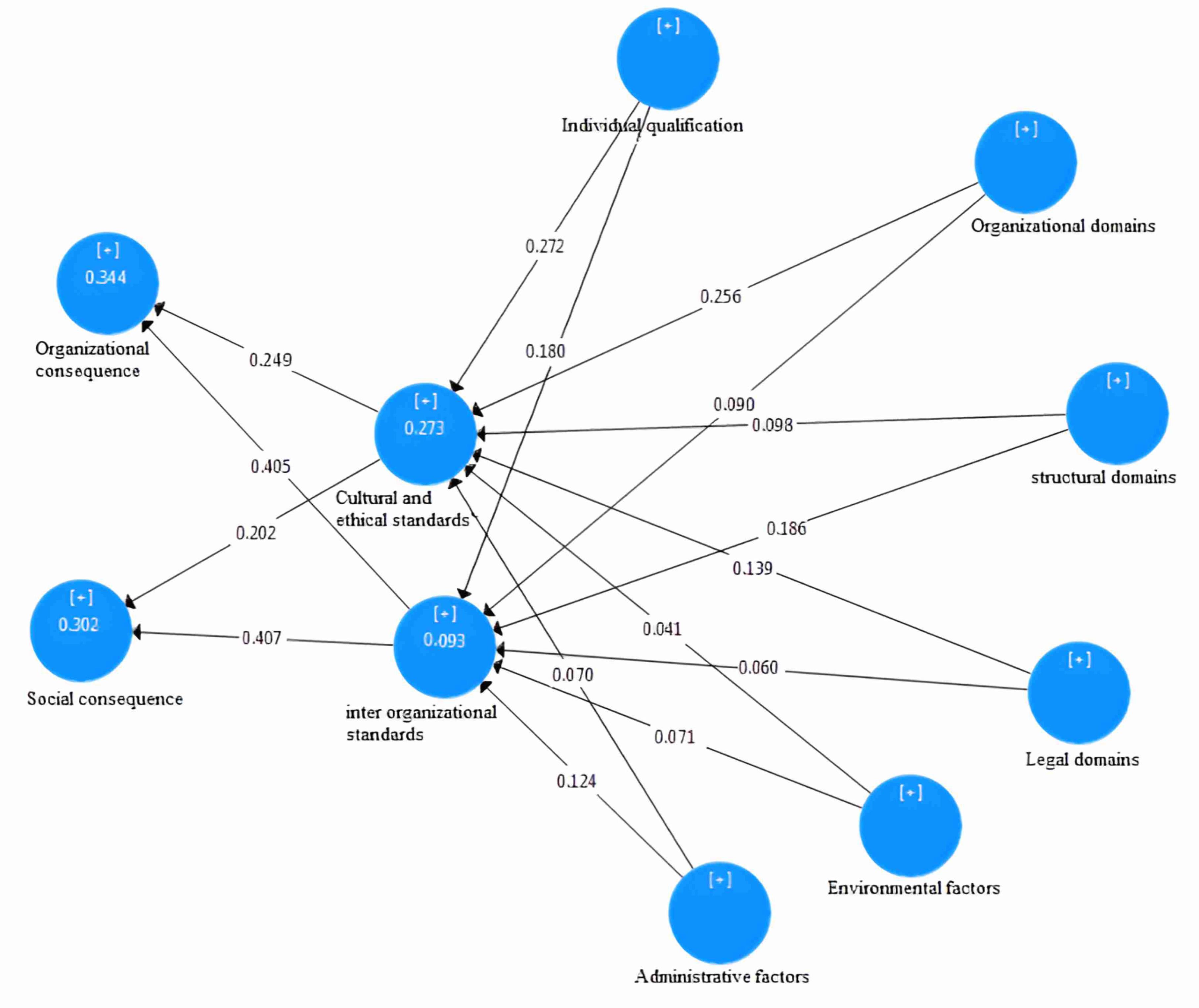
Figure 1.
Validation of the model using the partial least squares method in standard estimation mode
.
Validation of the model using the partial least squares method in standard estimation mode
To assess the significance of the relationships among the model variables, the bootstrap method was employed, providing the t statistic. At a 5% significance level, if the bootstrapping statistic exceeds 1.96, the observed correlations are deemed significant. Figure 2 displays both the t statistic and bootstrapping value for evaluating relationship significance.
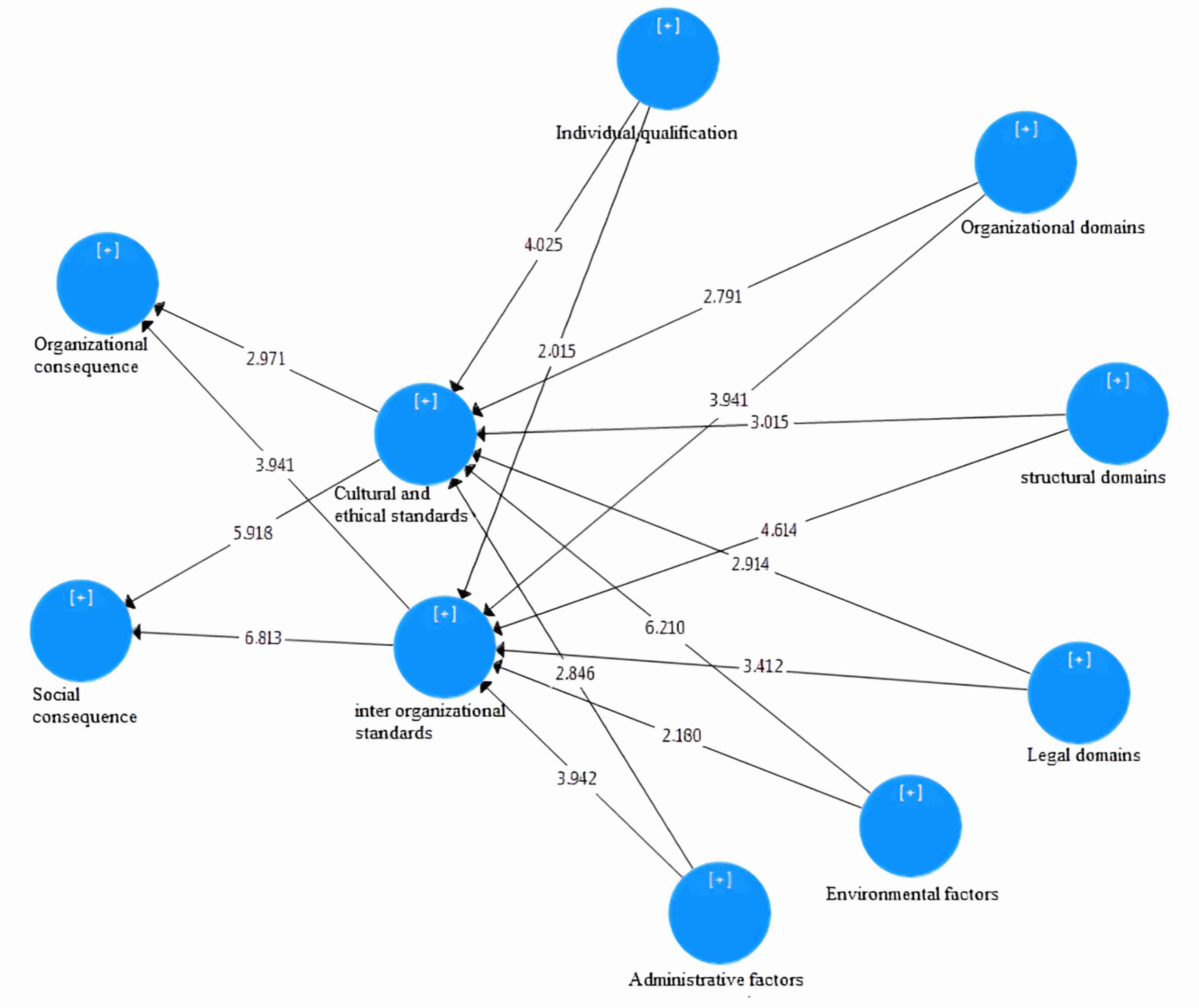
Figure 2.
Significance of variable relationships using the partial least squares method with bootstrapping
.
Significance of variable relationships using the partial least squares method with bootstrapping
SEM comprises two components: the measurement model and the structural model. Model variables are categorized as latent and manifest variables, with latent variables being utilized at various levels. The measurement model section includes indicators for each dimension alongside the dimension itself, examining the relationships between indicators and dimensions. In the structural model section, all structures mentioned in the primary model of the research are outlined, emphasizing the correlation between structures and their relationships.18 To evaluate the overall fit of the model, test hypotheses, and examine correlations, various techniques such as path coefficients testing, R2 recognition coefficient criteria, Q2 predictive power coefficient, goodness-of-fit (GOF) index, and T-value coefficients are employed. Additionally, to ensure validity and reliability, measures like Cronbach’s alpha coefficient, convergent validity (AVE), and composite reliability (CR) of the questionnaire are determined using SmartPLS software.
To assess the adequacy of the measurement model, we employed indicators of reliability, convergent validity, and divergent validity. Reliability serves as a metric for internal consistency and is gauged through three key factors: factor loadings, Cronbach’s alpha, and composite reliability. While Cronbach’s alpha has traditionally been utilized as a benchmark for variable reliability, the PLS method introduces a more contemporary metric known as composite reliability to evaluate the same.
Consequently, both of these metrics were utilized in the current study to enhance the assessment of reliability. If the combined reliability score for each variable surpasses 0.7, it signifies satisfactory internal consistency within the model; conversely, a score below 0.6 indicates inadequate reliability.19 Convergent validity, as indicated by the average variance extracted (AVE), serves as a benchmark for the measurement model’s adequacy. The AVE represents the average amount of variance shared between a variable and its respective indicators. Essentially, it reflects the extent of correlation between a variable and its indicators—a higher correlation implies better model fit. A threshold value of 0.4 is deemed critical, with an AVE exceeding this threshold indicative of acceptable convergent validity.19 Table 2 displays the model’s convergent validity, composite reliability, and Cronbach’s alpha.
Table 2.
Validity and reliability assessment for the measurement model
|
Indicators
|
Convergent validity (AVE)
|
Composite reliability (CR)
|
Cronbach's alpha
|
| Structural domains |
0.711 |
0.970 |
0.966 |
| Legal domains |
0.808 |
0.927 |
0.879 |
| Organizational domains |
0.735 |
0.951 |
0.939 |
| Individual qualification |
0.844 |
0.942 |
0.908 |
| Environmental factors |
0.500 |
0.855 |
0.802 |
| Administrative factors |
0.564 |
0.838 |
0.744 |
| Cultural and ethical standards |
0.619 |
0.829 |
0.700 |
| Interorganizational standards |
0.650 |
0.943 |
0.930 |
| Organizational consequence |
0.650 |
0.844 |
0.723 |
| Social consequence |
0.817 |
0.930 |
0.888 |
| Organizational trust based on professional ethics |
0.798 |
0.922 |
0.873 |
Based on Table 2, the results indicate that all dimensions have obtained a Cronbach’s alpha higher than 0.7, demonstrating good reliability in the research model. Additionally, the reliability for all dimensions exceeds 0.7. Moreover, the convergent validity for all dimensions surpasses 0.4. Following the given criteria, it can be concluded that the proposed model meets the required standards.
Evaluation of the structural model involved measuring the validity and reliability of the measurement model. This was followed by an assessment of the relationships between the underlying variables. The evaluation criteria used in this research included the significance coefficient (T-values), detection coefficient (R2), and predictive power coefficient (Q2). Table 3 presents the R2 and Q2 values for reference.
Table 3.
Results of fitting the structural model using the Q2 and R2 method
|
|
Cultural and ethical standards
|
interorganizational standards
|
Organizational consequence
|
Social consequence
|
| Q2 |
0.742 |
0.689 |
0.758 |
0.690 |
| R2 |
0.472 |
0.466 |
0.564 |
0.506 |
Based on the data presented in the table, the recognition coefficient (R2) for the endogenous structures within the research model is deemed favorable. This indicates that the coefficients’ values are acceptable across all instances. Additionally, the positive values of the Q2 index for all cases signify a good fit for the model.
Overall model fit: The GOF index assesses the overall model fit by considering both the measurement and structural model components.
Relationship 1
The calculated value of the goodness of fit in this study is equal to 0.01, which falls into the category of “weak” based on the classification introduced by Wetzles et al.20
Relationship 2
The mean value of the coefficient of determination index, denoted as (R2), is 0.719.
Relationship 3
Average values of redundancy index (Commonality) = 0.502
Relationship 4
The GOF index is 0.601, indicating that the model fits well.
Upon evaluating the adequacy of the measurement models, structural model, and general model, the research questions can be addressed, leading to the discovery of research findings. This section comprises two components: significant coefficients (T-value) and standardized factor loading coefficients or path coefficients related to the research hypotheses outlined in Table 4. The results of Table 4 show that the positive and significant impact of each of the independent variables on the dependent variables is confirmed.
Table 4.
Summary of the structural component results in the model (relationships among model variables)
|
Independent variable
|
The dependent variable
|
Factor load
|
t statistic
|
| Structural domains |
Cultural and ethical standards |
0.098 |
3.015 |
| Legal domains |
Cultural and ethical standards |
0.139 |
2.914 |
| Environmental factors |
Cultural and ethical standards |
0.041 |
6.210 |
| Administrative factors |
Cultural and ethical standards |
0.070 |
2.846 |
| Organizational consequence |
Cultural and ethical standards |
0.256 |
2.791 |
| Individual qualification |
Cultural and ethical standards |
0.272 |
4.025 |
| Structural domains |
interorganizational standards |
0.186 |
4.614 |
| Legal domains |
interorganizational standards |
0.060 |
3.412 |
| Environmental factors |
interorganizational standards |
0.071 |
2.015 |
| Administrative factors |
interorganizational standards |
0.124 |
1.994 |
| Organizational consequence |
Cultural and ethical standards |
0.090 |
2.791 |
| Individual qualification |
Cultural and ethical standards |
0.180 |
4.025 |
| Cultural and ethical standards |
Organizational consequence |
0.249 |
2.971 |
| interorganizational standards |
Organizational consequence |
0.405 |
3.941 |
| Cultural and ethical standards |
Social consequence |
0.202 |
5.918 |
| Interorganizational standards |
Social consequence |
0.407 |
6.813 |
Discussion
Based on the results obtained from the paradigmatic model derived from this research, organizational trust based on professional ethics in the healthcare system can be described as a comprehensive and complex framework comprising multiple factors and layers. Initially, the model considers causal conditions including structural domains (such as conflicts of interest, distrust, disorder, inappropriate culture, injustice, and managerial challenges) and legal domains (such as law evasion, ambiguity resolution, ethical accountability, and legal transparency). The model then examines contextual conditions, which include organizational processes (such as competition, organizational culture, training, appropriate communications and interactions, mutual trust, and management style) and individual competencies (such as proficiency, work conscience, discipline, honesty, integrity, respect for others’ rights, participatory spirit, accountability, risk-taking, positive mindset, and responsibility). Additionally, it takes into account environmental and administrative factors such as globalization, government macro policies, media and societal culture, technology and innovation, non-discrimination, absence of favoritism, and organizational culture in the healthcare system. The model also proposes strategies and actions in the areas of cultural and ethical standards, such as setting standards, advertising, observing fairness, adherence to organizational value principles, compliance with professional ethical charters, and strengthening spiritual culture. It also suggests intra-organizational standards like appropriate role modeling, employee recognition, strategic coordination, evaluation, knowledge sharing, delegation of authority, rule of law, fair payment mechanisms, compassionate leadership, and employee support. Finally, the model examines its outcomes at both organizational and social levels. At the organizational level, outcomes include improved performance, reduced conflict, decreased turnover, organizational vitality, increased self-confidence, sustainable competitive advantage, efficiency and effectiveness, administrative health, meritocracy, employee satisfaction, increased productivity and motivation, and enhanced organizational quality. At the social level, outcomes encompass increased public trust, improved organizational public image, institutionalization of ethical values, social commitment, improved public relations, public peace of mind, justice, improved service quality, public benefit, and enhanced community health. This model emphasizes that building organizational trust based on professional ethics principles is a dynamic and continuous process that requires attention to all mentioned factors and understanding the effective interaction between them, potentially leading to overall improvement in healthcare system performance.
Therefore, in general, it can be stated that: Trust plays a vital and multidimensional role in the healthcare system, exerting extensive influences on all aspects of healthcare. This key element is essential in creating a positive work environment, ensuring patient safety and satisfaction, and enhancing service quality. Healthcare organizations that prioritize trust and ethical standards are not only more successful in attracting and retaining competent managers, specialists, and staff, but also contribute to alleviating patients’ pain and providing peace of mind to their families by improving service quality. The expansion of trust based on professional ethics directly impacts employee satisfaction and commitment, which in turn leads to increased productivity, reduced financial costs, and improved service quality. This becomes particularly crucial in the healthcare system, which deals with people’s lives, psyche, and health. Trust in such systems not only affects patient treatment outcomes and overall organizational performance but also plays a role at a broader societal level. Through fulfilling social commitments and enhancing the organization’s public image, organizational trust leads to the promotion of justice, improvement of social communications, increase in public confidence and peace of mind, and ultimately contributes to the overall good and benefit of society. Alongside trust, professional ethics is also a key concept in the healthcare system, the necessity of which is evident to all. All individuals working in this field, from managers to specialists and staff, are expected to adhere to high ethical standards, including commitment to patient safety, maintaining confidentiality, and respecting patient autonomy. Adherence to professional ethics principles not only helps strengthen trust between patients and healthcare providers but also leads to improved treatment outcomes and enhanced organizational reputation. Furthermore, commitment to professional ethics increases employees’ sense of belonging and dedication to the organization. Overall, the combination of organizational trust and professional ethics provides the essential foundations for an efficient, humane, and responsive healthcare system that not only delivers high-quality services but also works towards improving the overall health and well-being of society.
The following researchers have delved into the factors influencing organizational trust and professional ethics, and how these factors are reflected in organizational performance: Atalay et al,10 Garib et al,11 Soni and Mehta,12 Basit and Duygulu,13 Bowen et al,14 Soleimani et al,21 Mehrgan and Sobhi,22 Haghgoo et al,15 Asadian et al,16 Hadavinejad and Sharifiasl.23
Comparison of the results obtained from the current study with those of previous research indicates that ethical and cultural standards have a notably positive impact on organizational outcomes, aligning with Bowen et al,14 Garib et al,11 and Mehrgan and Sobhi.20 The research findings demonstrate that administrative factors and individual qualifications positively influence internal standards, which echoes the results of Atalay et al,10 Soni and Mehta,12 Additionally, individual qualifications were found to have a positive and significant effect on organizational outcomes, consistent with the findings of Hadavinejad and Sharifiasl.23
Among the limitations of the study, we can mention the breadth and scope and different models of organizational trust and the time-consuming nature of their investigation, the honesty of the respondents to the research questions, the bias of the respondents’ perception of the questionnaire questions, the bias of the researcher in the qualitative aspect of the research, and the difficulty of communicating to obtain information from managers.
To create a solid foundation, strengthen positive effects among stakeholders, and increase the efficiency of organizational trust-building strategies that are rooted in professional ethics in the health care system, the following recommendations are suggested: Identifying the factors affecting the creation of trust and strengthening it, strengthening the interaction between employees and managers., having integrity and adhering to ethical agreements, providing ways for professional growth and development by strengthening commitment and long-term development of employees, encouraging independence in work practices to stimulate creativity, collecting feedback from employees on unnecessary rules and regulations, promoting ethics training Medicine by integrating Iranian-Islamic values, assessing needs, pathologies and promoting values and professional ethics in the framework of creating and monitoring the supervisory system of higher health education, compiling ethical standards and guidelines in medical education, establishing an ethical evaluation system in organizations, improving the system Salaries based on people’s work performance and ethical behavior to strengthen trust in the organization, giving priority to hiring employees with education, skills and work experience related to organizational values and professional ethics. Restoring and fostering trust requires a dedicated effort from organizational managers. They must take proactive steps to uphold values like respecting employees, fostering an environment conducive to open communication and support, and building trust among team members to promote organizational learning. By doing so, managers can influence the organization’s momentum and drive positive change. Restoring and fostering trust requires a dedicated effort from organizational managers.
Conclusion
After examining the relationships between key research structures in the collected data from managers, experts, and employees in the health system, it was found that the observed path coefficient and t statistic values (bootstrapping) of the variables indicate that all factor loadings at the 95% confidence level were above 1.96. This suggests a significant relationship between visible variables (concepts) and latent variables (categories), with all factor loadings being verified. Furthermore, the results reveal that structural domains, legal domains, environmental factors, administrative factors, organizational consequences, and individual qualifications exhibit a positive and significant correlation with cultural and ethical standards as well as inter-organizational standards. On the flip side, cultural and ethical standards, as well as inter-organizational standards, exhibit a positive and significant correlation with both organizational and social outcomes. The study’s findings indicate that causal conditions play a crucial role in influencing the central phenomenon, contextual and intervening conditions, organizational strategies, and the ramifications of organizational trust within the healthcare sector when viewed through a professional ethics lens. The outcome of this study, showcasing a comprehensive organizational trust model utilizing a professional ethics approach in the healthcare system, is presented in Figure 3, marking a significant contribution. This model meticulously outlines the components and indicators of organizational trust tailored to Iran’s healthcare system, encompassing all relevant dimensions and components.
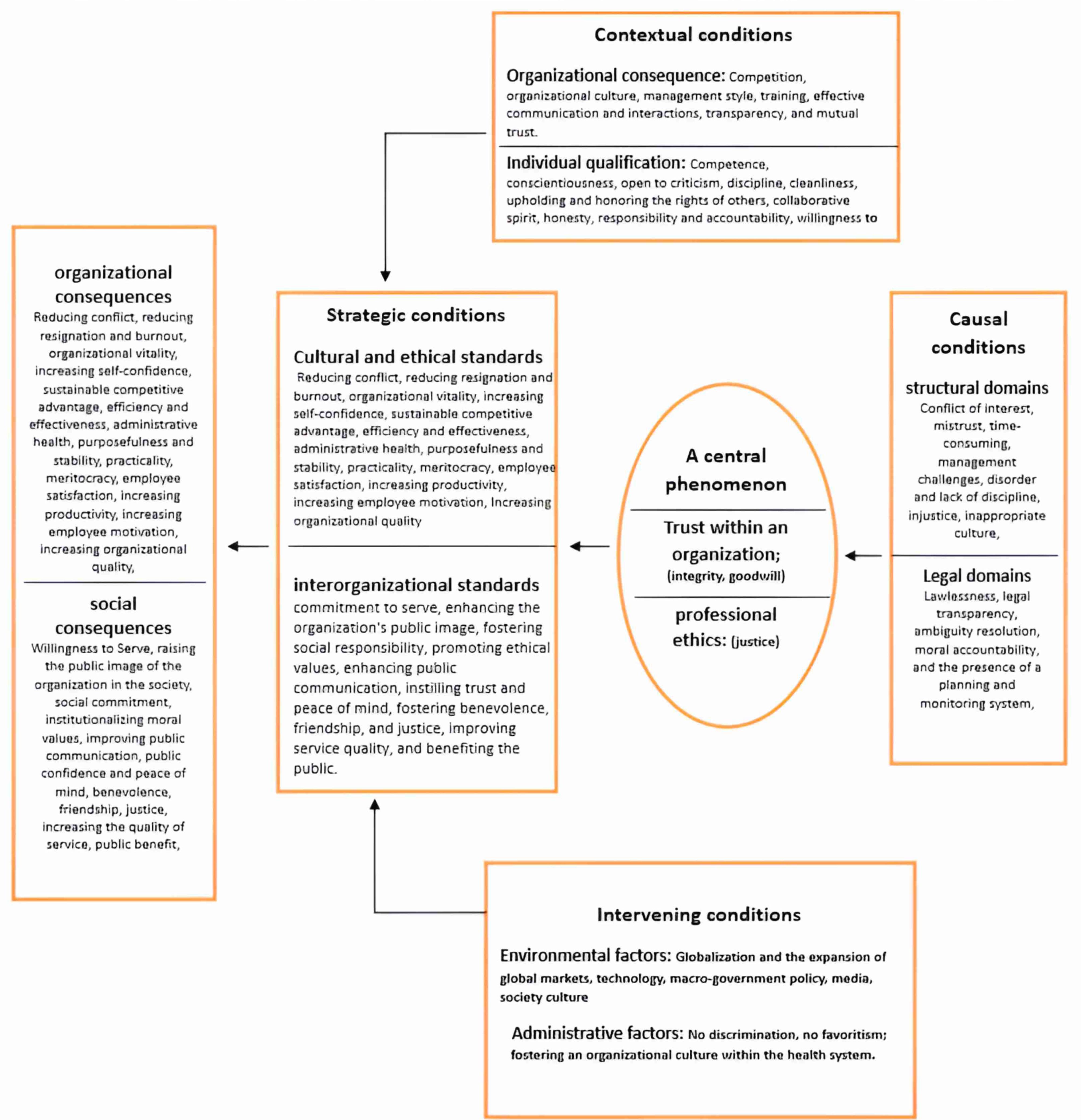
Figure 3.
The comprehensive model of organizational trust with the approach of professional ethics in the health system
.
The comprehensive model of organizational trust with the approach of professional ethics in the health system
Acknowledgments
This excerpt is derived from doctoral thesis number 162281984 and has been authorized officially by the Research Council of Bonab Azad University. We extend our sincere appreciation to all managers, experts, employees, and faculty members of universities of medical sciences who collaborated and contributed to this research.
Competing Interests
The authors declare no conflict of interest
Ethical Approval
Not applicable.
References
- Birden H, Glass N, Wilson I, Harrison M, Usherwood T, Nass D. Defining professionalism in medical education: a systematic review. Med Teach 2014; 36(1):47-61. doi: 10.3109/0142159x.2014.850154 [Crossref] [ Google Scholar]
- Pourhaydari R, Sameri M, Hassani M, Mortazanejad N. Structural relationships between organizational trust, professional ethics, organizational structure with school effectiveness with mediating role of teachers’ performance evaluation. Journal of Instruction and Evaluation 2019;12(47):93-116. [Persian].
- Saunders MNK, Thornhill A. Organisational justice, trust and the management of change. Pers Rev 2003; 32(3):360-75. doi: 10.1108/00483480310467660 [Crossref] [ Google Scholar]
- Fulmer CA, Gelfand MJ. At what level (and in whom) we trust: trust across multiple organizational levels. J Manage 2012; 38(4):1167-230. doi: 10.1177/014920631243932 [Crossref] [ Google Scholar]
- Khanbashi M, Zahedi S, Alvani SM. Accountability: the basis for public trust enhancement. Quarterly of Order and Security Guards 2011;4(2):25-50. [Persian].
- Wynia MK, Papadakis MA, Sullivan WM, Hafferty FW. More than a list of values and desired behaviors: a foundational understanding of medical professionalism. Acad Med 2014; 89(5):712-4. doi: 10.1097/acm.0000000000000212 [Crossref] [ Google Scholar]
- Shafighi F, Kalantari M, Zolfaghari Zaferani R. The effect of professional ethics on teachers’ performance and job motivation with the mediating role of religiosity in work. Research in Educational Systems 2017;12(Special Issue):985-1008. [Persian].
- Salam A, Yousuf R, Islam MZ, Yesmin F, Helali AM, Alattraqchi AG. Professionalism of future medical professionals in Universiti Sultan Zainal Abidin, Malaysia. Bangladesh J Pharmacol 2013; 8(2):124-30. doi: 10.3329/bjp.v8i2.14158 [Crossref] [ Google Scholar]
- Mohammadi T, Bohloli N, Beykzad J, Rahimi G. Develop a Comprehensive Performance Management Model Based on Ethics Approach in Government Organizations. Ethics Sci Technol 2021;16(2):148-55. [Persian].
- Atalay M, Birincioğlu N, Acuner T. Effect of perceived organizational support and organizational trust on young academics’ organizational commitment. Argum Oecon 2022; 48(1):201-33. doi: 10.15611/aoe.2022.1.09 [Crossref] [ Google Scholar]
- Garib M, Qashqaizadeh N, Omidian F. Creating a framework for understanding the factors influencing the evolution of nurses’ professionalism. Islamic Lifestyle with a Focus on Health 2023;6(4):208-18. [Persian].
- Soni D, Mehta P. Manifestation of internal CSR on employee engagement. Indian J Ind Relat 2020; 55(3):441-59. [ Google Scholar]
- Basit G, Duygulu S. Nurses’ organizational trust and intention to continue working at hospitals in Turkey. Collegian 2018; 25(2):163-9. doi: 10.1016/j.colegn.2017.05.003 [Crossref] [ Google Scholar]
- Bowen SA, Hung-Baesecke CJ, Chen YR. Ethics as a precursor to organization–public relationships: building trust before and during the OPR model. Cogent Soc Sci 2016; 2(1):1141467. doi: 10.1080/23311886.2016.1141467 [Crossref] [ Google Scholar]
- Haghgoo M, Daneshfard K, Tabibi SJ. Designing a pattern for development professional ethics of government organization: health system of Iran. J Health Adm 2017;21(72):99-112. [Persian].
- Asadian S, Rabiei M, Qasimzadeh A. The relationship between professional ethics and organizational trust with teachers’ psychological empowerment. Quarterly Scientific Journal of Applied Ethics Studies 2016; 12(44):165-95. doi: 10.22081/jare.2017.45016.[Persian] [Crossref] [ Google Scholar]
- Hair JF, Hult GTM, Ringle CM, Sarstedt M. A Primer on Partial Least Squares Structural Equation Modeling. Sage, Thousand Oaks, CA: 2014.
- Talebi K, Davari A, Dehghan Najmabadi A. The effect of intellectual capital on entrepreneurial opportunity recognition. Journal of Management Studies in Development & Evaluation 2013;23(71):19-48. [Persian].
- Budaghi Khajeh Nobar H, Esgandari K, Rostamzadeh R. The effect of managers’ competitive intelligence on modernization of small industries. Productivity Management 2016;10(37):81-106. [Persian].
- Wetzels M, Odekerken-Schröder G, Van Oppen C. Using PLS path modeling for assessing hierarchical construct models: Guidelines and empirical illustration. MIS quarterly. 2009: 177-95.
- Soleimani M, Zavvar T, Daneshvae Heris Z, Khadivi A, Talebi B. Characteristics of professional ethics in the health education system of northwestern medical universities: a qualitative study. Depiction of Health 2022; 13(2):198-209. doi: 10.34172/doh.2022.27 [Crossref] [ Google Scholar]
- Mehrgan F, Sobhi E. Analysis of the structural relationship between the organizational trust with the self-efficiency and professional ethics among nurses. Quarterly Journal of Nersing Management 2020;8(4):41-53. [Persian].
- Hadavinejad M, Sharifiasl M. Consequences of interpersonal trust as an ethical component in organization. Ethics Sci Technol 2015;10(2):52-62. [Persian].