Res Dev Med Educ. 13:32.
doi: 10.34172/rdme.33262
Narrative Review
Optimizing interprofessional education: Integrating a portfolio-based approach in undergraduate curriculum
Sangeetha Kandasamy Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Writing – original draft, 1, * 
Shivkumar Gopalakrishnan Conceptualization, Investigation, Methodology, Writing – original draft, Writing – review & editing, 2 
Harikrishnan Elangovan Data curation, 3 
Satish Kumar Rajasekaran Resources, 2 
John Humphrey Victor Gilbert Supervision, Writing – review & editing, 4 
Author information:
1Department of Biochemistry, Government Villupuram Medical College & Hospital,Villupuram 605602,Tamilnadu, India
2Department of Internal Medicine, Government Villupuram Medical College & Hospital,Villupuram 605602,Tamilnadu, India
3Department of Peadiatrics, Indira Gandhi Medical College and Research Institute, Kathirkamam, Puducherry, 605 009, India
4Department of Speech Sciences, UBC Emeritus College, University of British Columbia, Vancouver, BC V6T 1Z4, Canada
Abstract
Background:
Interprofessional education (IPE) is the need of the hour for any undergraduate curriculum to build interprofessional communication skills, adapt teamwork, and role clarity of various healthcare professionals in the early stage of a learning period. The outcome will improve patient safety and quality of care through a holistic approach by addressing lacunae in interprofessional collaboration.
Methods:
To describe the steps to implement the IPE curriculum and evaluation of learners’ activity through an IPE portfolio.
Results:
Sensitization of IPE curriculum among various health professional faculties, and students. Develop core team facilitators, and construct lesson plans and assessments. The IPE portfolio will be used as a reliable and effective tool for formative assessment including authentic, real-world examples of learner’s work.
Conclusion:
This paper communicates undergraduates’ reflection practices in patient care stimulate critical thinking, deep and lifelong learning, and, facilitating from novice to mastery levels are achieved through integrated and aligned with IPE curriculum and portfolios-based assessment tool.
Keywords: Interprofessional education, Curriculum, Portfolio-based assessment, Reflective process
Copyright and License Information
© 2024 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, as long as the
original authors and source are cited. No permission is required from the authors or the publishers.
Funding Statement
No financial support was received for the research, authorship, or publication of this article.
Introduction
Health organizations worldwide implemented a universal interprofessional education (IPE) plan in 1988. IPE is defined as “Occasions when members or students of two or more professions: learn with, from, and about each other, to improve collaboration and the quality of care and services.” The Centre for Interprofessional Education (UK) Definition (2002, modified 2017)
IPE is a firmly established necessity for health and social care professionals to possess a set of skills that extend beyond their curriculum. In many medical educational systems worldwide, undergraduate education is inclined to operate within silos, with each profession conducting its teaching-learning activities (WHO 2010). This isolated approach often results in healthcare professionals graduating with limited interprofessional communication, collaboration, and teamwork performance skills, hindering their ability to adapt to challenges and respond adequately to patients’ healthcare needs. The importance of IPE arises from the fact that coordination of various healthcare services is essential to meet the manifold requirements of patients and reduce medical errors, and hospital readmission rates, ultimately supporting the achievement of the Triple Aim of healthcare1,2,3 (Figure 1).
Figure 1.
Interprofessional competencies will achieve the above triple aim
.
Interprofessional competencies will achieve the above triple aim
Needs of IPE in undergraduate curriculum
IPE programs in the UK and US-based medical centers are committed to achieving health care improvement. This initiative has been adopted by different universities, professional associations, and healthcare institutions, who also address the need to provide IPE for their learners.4 An interprofessional collaborative approach enables students to understand each other’s roles, standpoints, and contributions to patient safety and the quality of care. The establishment of IPE should be in line with ethical principles, emphasizing the importance of integrity, respect, and professionalism. Novices should learn to acknowledge the ethical dimensions of interprofessional collaboration, including patient confidentiality, shared decision-making, and cultural capacity. IPE programs reinforce early learning experiences (pre-qualification stages) throughout their career diminishing the negative effects of professional isolation like hostile stereotyping, and improving post-qualification work practices.5 IPE should include experiential learning methods, such as simulated patient care scenarios, blended learning, shadow learning, problem-based learning, collaborative projects, and interprofessional training programs. These activities provide students with the hands-on experience to apply interprofessional skills and enhance their critical thinking ability to work together in real-world health and social care settings.
Assessment methods in IPE outcomes should be mapped to evaluate both individual and team performance. This may include peer assessments, self-reflection, and opinions by faculty members. Regular feedback can help students realize their strengths and scope for improvement in interprofessional collaboration.6
Implementation at health care institutions
Interprofessional Collaborative Competencies (IPEC 2023) updated four core competencies as an integral part of interprofessional collaboration and emphasized that patient and family-centered care should be provided keeping in mind the needs of the community and population. The four core competencies are (1) Roles & responsibilities for collaborative practice, (2) Values/ethics for interprofessional practices, (3) Interprofessional communication practices, (4) Interprofessional teamwork and team-based practice.1
The development of interprofessional collaborative competencies developed both by IPEC and the Canadian Interprofessional Health Collaborative (CIHC, 2024) is important to move out with profession-specific educational efforts to engage students of different professions in interactive learning with each other. At the level of tertiary care, most institutes have more than one course, and easy to implement the experiential learning of IPE. The objectives of IPE activity can be achieved from the time of diagnosis, investigations, treatment, and prevention of chronic and acute diseases, which require the collaborative efforts of various health and social care workers. Undergraduate teaching institutions specially focussed on healthcare education have the responsibility to teach and train students to respond to challenges and patients’ healthcare needs in a collaborative working environment. The progression pathway to achieve the IPE goals is explained (Figure 2).
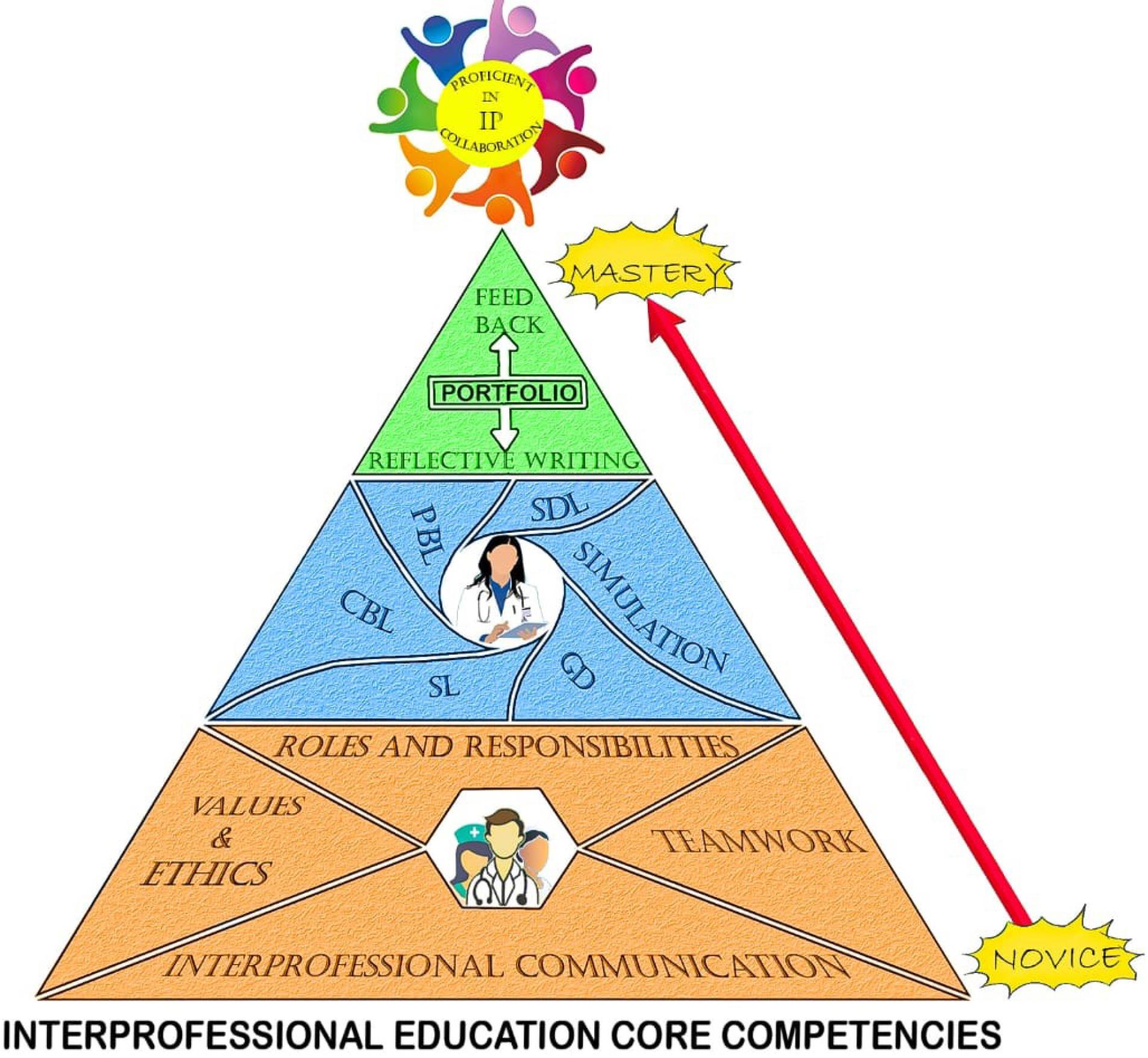
Figure 2.
Interprofessional education progression pathways
.
Interprofessional education progression pathways
The steps to implement IPE at the institutional level
The learning phases of the IPE curriculum for health professional learners, progressing from exposure to mastery, guide learners on a journey from novice to expert, preparing them to apply their skills effectively in real-world settings (Table 1).
Table 1.
Learningphase of the IPE curriculum from exposure to mastery
7-10
|
Phase
|
Definition
|
| Exposure phase |
The first phase of IPE is to prepare the organization and intended learners to come together with students who represent other health professions. This phase occurs through orientation programs, small group discussions, and social activities. |
| Immersion Phase |
The middle phase warrants collaborative interactions that help learners focus on learning with, from, and about each other’s profession. This phase also helps the student understand interprofessional values and ethics along with role clarification which are deemed vital ingredients for effective teamwork and collaboration in healthcare. This happens through case discussions, team meetings, bedside rounds, and simulation-based teaching. |
| Mastery Phase |
The phase of integration of critical thinking and problem-solving in complex real-world situations. |
-
Create core team members from various professional educators.
-
Sensitization of IPE among facilitators & undergraduate students (Exposure).
-
Develop a lesson plan for IPE as an integral part of their curriculum (Figure 3).
-
Monitor the student’s activity in the portfolio with feedback. (Immersion).
-
Assess the learning process and look forward to the long-term outcome of patient safety (Mastery).7-10
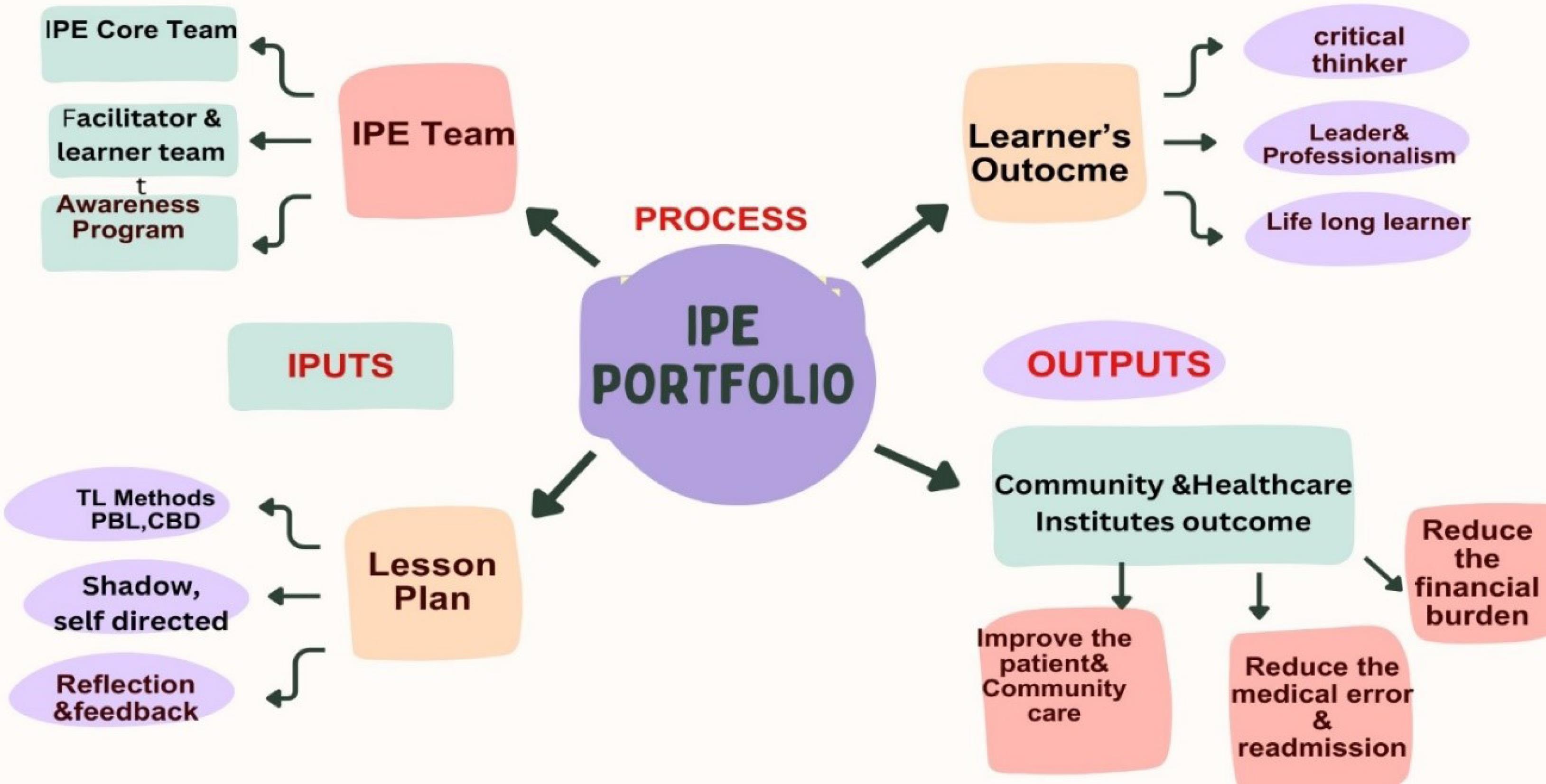
Figure 3.
CIPP model of IPE portfolio
.
CIPP model of IPE portfolio
Factors influencing the implementation of IPE
-
Health professionals need to know “how to explore, benefit from, and collaborate with other professionals”. It is a fresh and demanding task, whether through formal or informal educational approaches.
-
Faculty development in IPE plays a key role in diminishing isolation, cultivating a collaborative facilitation style, as well as providing opportunities for faculty to share knowledge, experiences, and ideas.
-
With organizational support and a dedicated group of facilitators short-term outcomes such as fostering positive attitudes, clarifying roles, and enhancing communication skills among learners can be achieved. In the long run, these efforts can contribute to the creation of an organizational culture where 100% patient safety is ensured.
Learning interprofessional education is a student-centered activity
IPE learning activity is learner-centered and works on a student engagement approach. Examining the program through the lens of the Contexts, Inputs, Processes, Products/outputs (CIPP) model across all event stages can facilitate the identification of and solution to barriers. Integration of this CIPP model into our IPE portfolio aims to improve evaluation and problem-solving ability. The primary input focus of the portfolio is the formation of IPE teams, and lesson plan development, as illustrated in Figure 3. The process of portfolio documentation culminates in optimizing outcomes for learners and the healthcare community.11
Each stage prompts the learner to examine their experiences through questions designed to incite deep and critical reflection.10 Achieving interprofessional competencies not only assures knowledge of IPE but also gives feedback with measurable evidence of learning. Thus, a portfolio represents measurable evidence of learning (assignments, case narration, observational checklist rating, documentation) and work experience. The work plan is based on experiential learning. Portfolio is a reliable and valid tool for formative and summative assessment. IPE portfolio is a continuous process wherein the faculty supervisor gives feedback to the student. This practice is highly recommended to reinforce the learning ability of the student.12,13
Evaluation of the IPE curriculum
Portfolios are powerful tools that can enhance this reflective practice. Reflection on one’s achievements, strengths, and weaknesses is a key component of adult learning. This process allows learners to better understand their learning styles, supporting self-directed learning by fostering reflection, self-assessment, goal-setting, continuous improvement of skills knowledge, and professional attitude. They provide a structured and personalized way for adult learners to take ownership of their learning process. As learners add artifacts, reflections, and examples of their work to their portfolios, instructors can track their development and understanding of the subject matter at the level of outcome evaluation by the Kirkpatrick model. There are four levels of evaluation for educational programs: reaction, learning, behavior, and result.14 No single comprehensive tool fully meets the diverse needs of assessing IPE competencies holistically. A Review of the National Centre for Interprofessional Practice and Education website highlights the availability of quantitative assessment tools for evaluating IPE competencies. Most of these tools focus on assessing outcomes at Kirkpatrick’s Level 3, emphasizing behavioral changes resulting from the educational intervention.15
Portfolio is less frequently used in pre-registration education across the health sciences. It is, however, useful with pre-registration students when they receive reflective feedback on their learning experience at Kirkpatrick level three. It shows the behavioral change in undergraduate students, grooming them to handle future teamwork, lifelong learning, and improvement of their communication skills16 (Figure 4).
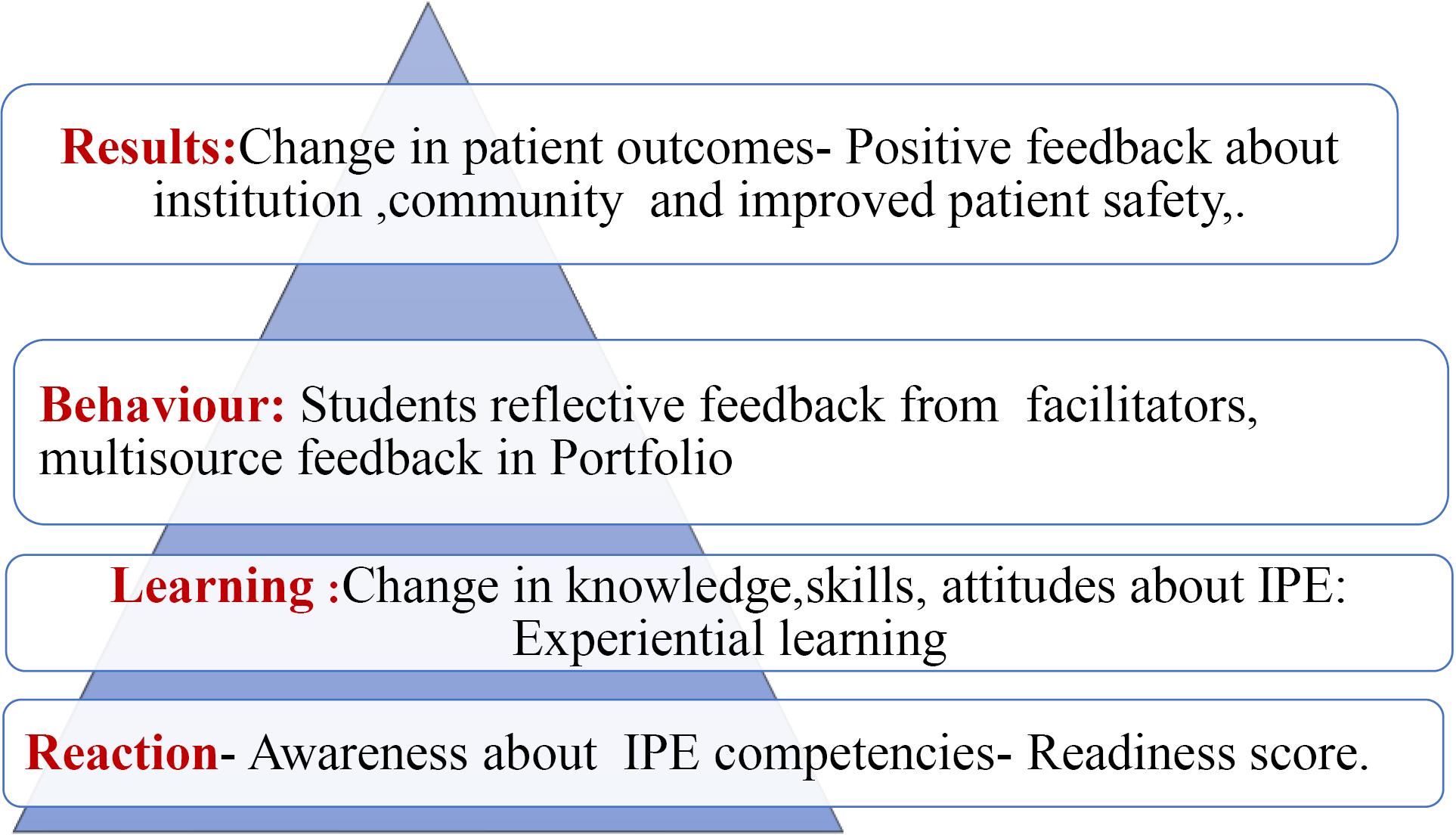
Figure 4.
Assessing the IPE curriculum implementation program using Kirpartick’s levels
.
Assessing the IPE curriculum implementation program using Kirpartick’s levels
Conclusion
IPE presents opportunities necessary for learners from different health and social care professions to learn about the knowledge, skills, and expertise of each person on the team for the team to function well. IPE emphasizes the patient-centered approach, concentrating on outcomes driven by real-world examples and student-centered learning processes. Self-assessment promotes independent learning and encourages learners to take responsibility for their educational journey, fostering a sense of ownership. This proactive learning process is accomplished through portfolio documentation which serves as a valuable tool.
Acknowledgements
The authors thank the faculty members of Manipal Academy of Higher Education -FAIMER International Institute for Leadership in Interprofessional Educationin Manipal, Udupi Dt., Karnataka - 576 104. India, for generously sharing their valuable knowledge about Interprofessional education.
Competing Interests
The authors declare no competing interest.
Ethical Approval
Ethical approval was not obtained and does not apply to this study.
References
- Interprofessional Education Collaborative (IPEC). IPEC Core Competencies for Interprofessional Collaborative Practice: Version 3. Washington, DC: IPEC; 2023.
- Hegde S, Gajre MP, Shah H, Soares NS. Interprofessional education and practice in an Indian setting. J Taibah Univ Med Sci 2017; 12(3):265-7. doi: 10.1016/j.jtumed.2016.08.005 [Crossref] [ Google Scholar]
- Ahmady S, Mirmoghtadaie Z, Rasouli D. Challenges to the implementation of interprofessional education in health profession education in Iran. Adv Med Educ Pract 2020; 11:227-36. doi: 10.2147/amep.S236645 [Crossref] [ Google Scholar]
- Barr H, Koppel I, Reeves S, Hammick M, Freeth D. Effective Interprofessional Education: Argument, Assumption and Evidence. Oxford: Blackwell; 2005.
- Kemp S, Brewer M. Early stages of learning in interprofessional education: stepping towards collective competence for healthcare teams. BMC Med Educ 2023; 23(1):694. doi: 10.1186/s12909-023-04665-8 [Crossref] [ Google Scholar]
- Reeves S. Why we need interprofessional education to improve the delivery of safe and effective care. Interface (Botucatu) 2016; 20(56):185-97. doi: 10.1590/1807-57622014.0092 [Crossref] [ Google Scholar]
- Charles G, Bainbridge L, Gilbert J. The University of British Columbia model of interprofessional education. J Interprof Care 2010; 24(1):9-18. doi: 10.3109/13561820903294549 [Crossref] [ Google Scholar]
- El-Awaisi A, Anderson E, Barr H, Wilby KJ, Wilbur K, Bainbridge L. Important steps for introducing interprofessional education into health professional education. J Taibah Univ Med Sci 2016; 11(6):546-51. doi: 10.1016/j.jtumed.2016.09.004 [Crossref] [ Google Scholar]
- Aldriwesh MG, Alyousif SM, Alharbi NS. Undergraduate-level teaching and learning approaches for interprofessional education in the health professions: a systematic review. BMC Med Educ 2022; 22(1):13. doi: 10.1186/s12909-021-03073-0 [Crossref] [ Google Scholar]
- Mohammed CA, Anand R, Saleena Ummer V. Interprofessional education (IPE): a framework for introducing teamwork and collaboration in health professions curriculum. Med J Armed Forces India 2021; 77(Suppl 1):S16-21. doi: 10.1016/j.mjafi.2021.01.012 [Crossref] [ Google Scholar]
- Stufflebeam DL. The CIPP model for program evaluation. In: Evaluation Models: Viewpoints on Educational and Human Services Evaluation. Dordrecht: Springer; 1983. p. 117-41. 10.1007/978-94-009-6669-7_7.
- Hermasari BK, Rahayu GR, Claramita M. How does portfolio assess interprofessional learning among medical and midwifery students?. Int J Eval Res Educ 2019; 8(3):392-400. doi: 10.11591/ijere.v8i3.20245 [Crossref] [ Google Scholar]
- Imafuku R, Kataoka R, Ogura H, Suzuki H, Enokida M, Osakabe K. What did first-year students experience during their interprofessional education? A qualitative analysis of e-portfolios. J Interprof Care 2018; 32(3):358-66. doi: 10.1080/13561820.2018.1427051 [Crossref] [ Google Scholar]
- Mukhalalati BA, Taylor A. Adult learning theories in context: a quick guide for healthcare professional educators. J Med Educ Curric Dev 2019; 6:2382120519840332. doi: 10.1177/2382120519840332 [Crossref] [ Google Scholar]
- Shrader S, Farland MZ, Danielson J, Sicat B, Umland EM. A systematic review of assessment tools measuring interprofessional education outcomes relevant to pharmacy education. Am J Pharm Educ 2017; 81(6):119. doi: 10.5688/ajpe816119 [Crossref] [ Google Scholar]
- Hean S, Craddock D, O’Halloran C. Learning theories and interprofessional education: a user’s guide. Learn Health Soc Care 2009; 8(4):250-62. doi: 10.1111/j.1473-6861.2009.00227.x [Crossref] [ Google Scholar]